Lancet:新冠肺炎患者出院半年后,76%新冠患者还至少有一个持续症状
时间:2022-10-13 15:58:35 热度:37.1℃ 作者:网络
1月9日发表在《柳叶刀》(The Lancet)上的一份研究显示,76%的新冠患者在出院6个月后仍有至少一个持续症状。其中,疲劳或肌肉无力(63%)是最常见的症状,睡眠障碍(26%)、焦虑和抑郁(23%)也频繁出现。本研究由武汉市金银潭医院、中日友好医院呼吸中心、国家呼吸医学中心和中国医学科学院病原生物学研究所共同完成。曹彬、张定宇和王健伟为共同通讯作者;黄朝林、黄立学、王业明、李霞、任丽丽、谷晓颖、康亮、郭丽和刘敏为共同第一作者。
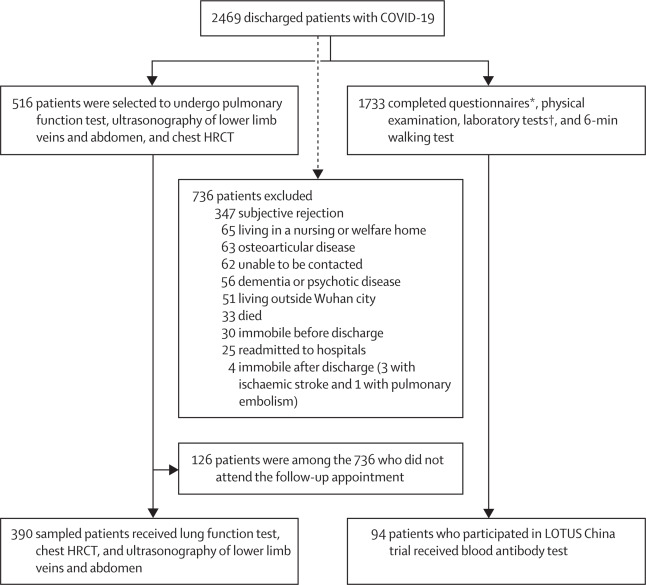
这项随访研究于2020年6月16日至9月3日期间完成,入选了2020年1月7日至5月29日期间自武汉市金银潭医院出院的1733例患者参加问卷调查、体格检查、实验室测试和6分钟的步行测试。患者的年龄中位数是57岁,其中男性897人(52%),女性836人(48%)。
研究人员对所有患者进行面对面访视,通过一系列问卷评估其症状和健康相关的生活质量。他们还接受了体格检查、实验室检查和评估患者耐力水平的6分钟步行实验。其中390例患者接受进一步包括肺功能评估在内的检查。此外,94例参与另外一个临床试验(LOTUS China)且完成急性期SARS-CoV-2抗体检测的患者在随访时再次进行抗体检测。
研究发现,在随访时76%(1265/1655)的患者报告仍有至少一个症状,63%(1038/1655)的患者报告出现疲劳或肌肉无力,26%(437/1655)的患者存在睡眠障碍,23%(367/1733)的患者报告出现焦虑或抑郁。
在390例进行肺功能检查的患者中,由于41例无法配合完成,最终349例完成了肺功能检查。住院时病情越重的患者中出现肺功能下降的情况更常见:7等级量表评分5-6分(住院期间接受机械通气治疗)的患者中,56%(48/86)出现肺弥散功能障碍,意味着氧气自肺泡向血流中的扩散能力下降。肺弥散功能障碍在7等级量表评分4分(住院期间接受氧疗)的患者中比例为29%(48/165),在评分3分(住院期间不接受氧疗)的患者中比例为22%(18/83)。
住院时病情更重的患者在6分钟步行试验(测量受试者于6分钟内步行的距离)中表现更差,7等级量表评分5-6分的患者中有29%未达到正常预计值的下限,然而该比例在3分患者中为24%,4分患者中为22%。
研究还发现部分患者在出院后出现肾脏问题。除了肺脏,COVID-19还会影响包括肾脏在内的其他器官。实验室检查发现,住院时肾功能正常的患者中有13%(107/822)在随访时出现肾功能异常。
| Total (n=1733) | Seven-category scale | OR or β (95% CI) | |||||
|---|---|---|---|---|---|---|---|
| Scale 3: not requiring supplemental oxygen (n=439) | Scale 4: requiring supplemental oxygen (n=1172) | Scale 5–6: requiring HFNC, NIV, or IMV (n=122) | Scale 4 vs 3 | Scale 5–6 vs 3 | |||
| Symptoms | |||||||
| Any one of the following symptoms | 1265/1655 (76%) | 344/424 (81%) | 820/1114 (74%) | 101/117 (86%) | OR 0·70 (0·52 to 0·96)* | OR 2·42 (1·15 to 5·08)* | |
| Fatigue or muscle weakness | 1038/1655 (63%) | 281/424 (66%) | 662/1114 (59%) | 95/117 (81%) | OR 0·74 (0·58 to 0·96)* | OR 2·69 (1·46 to 4·96)* | |
| Sleep difficulties | 437/1655 (26%) | 116/424 (27%) | 290/1114 (26%) | 31/117 (26%) | OR 0·92 (0·71 to 1·21) | OR 1·15 (0·68 to 1·94) | |
| Hair loss | 359/1655 (22%) | 93/424 (22%) | 238/1114 (21%) | 28/117 (24%) | OR 0·99 (0·74 to 1·31) | OR 1·17 (0·67 to 2·04) | |
| Smell disorder | 176/1655 (11%) | 55/424 (13%) | 107/1114 (10%) | 14/117 (12%) | OR 0·69 (0·48 to 1·00) | OR 0·90 (0·43 to 1·87) | |
| Palpitations | 154/1655 (9%) | 45/424 (11%) | 96/1114 (9%) | 13/117 (11%) | OR 0·86 (0·58 to 1·28) | OR 1·31 (0·61 to 2·80) | |
| Joint pain | 154/1655 (9%) | 51/424 (12%) | 86/1114 (8%) | 17/117 (15%) | OR 0·56 (0·38 to 0·83)* | OR 0·74 (0·36 to 1·50) | |
| Decreased appetite | 138/1655 (8%) | 42/424 (10%) | 85/1114 (8%) | 11/117 (9%) | OR 0·84 (0·56 to 1·27) | OR 1·56 (0·71 to 3·43) | |
| Taste disorder | 120/1655 (7%) | 37/424 (9%) | 75/1114 (7%) | 8/117 (7%) | OR 0·84 (0·54 to 1·30) | OR 0·80 (0·32 to 2·02) | |
| Dizziness | 101/1655 (6%) | 32/424 (8%) | 60/1114 (5%) | 9/117 (8%) | OR 0·77 (0·48 to 1·22) | OR 0·95 (0·39 to 2·31) | |
| Diarrhoea or vomiting | 80/1655 (5%) | 27/424 (6%) | 48/1114 (4%) | 5/117 (4%) | OR 0·71 (0·42 to 1·22) | OR 0·39 (0·11 to 1·42) | |
| Chest pain | 75/1655 (5%) | 19/424 (4%) | 46/1114 (4%) | 10/117 (9%) | OR 0·94 (0·52 to 1·67) | OR 2·55 (0·99 to 6·62) | |
| Sore throat or difficult to swallow | 69/1655 (4%) | 20/424 (5%) | 44/1114 (4%) | 5/117 (4%) | OR 0·91 (0·50 to 1·65) | OR 1·21 (0·40 to 3·73) | |
| Skin rash | 47/1655 (3%) | 16/424 (4%) | 27/1114 (2%) | 4/117 (3%) | OR 0·64 (0·32 to 1·26) | OR 0·71 (0·18 to 2·87) | |
| Myalgia | 39/1655 (2%) | 11/424 (3%) | 24/1114 (2%) | 4/117 (3%) | OR 0·80 (0·38 to 1·69) | OR 1·72 (0·47 to 6·27) | |
| Headache | 33/1655 (2%) | 10/424 (2%) | 20/1114 (2%) | 3/117 (3%) | OR 0·76 (0·35 to 1·69) | OR 1·53 (0·36 to 6·52) | |
| Low grade fever | 2/1655 (<1%) | 1/424 (<1%) | 1/1114 (<1%) | 0 | NA | NA | |
| mMRC score | |||||||
| 0 | 1196/1615 (74%) | 323/425 (76%) | 802/1079 (74%) | 71/111 (64%) | NA | NA | |
| ≥1 | 419/1615 (26%) | 102/425 (24%) | 277/1079 (26%) | 40/111 (36%) | OR 1·11 (0·84 to 1·46) | OR 2·15 (1·28 to 3·59)* | |
| EQ-5D-5L questionnaire † | |||||||
| Mobility: problems with walking around | 113/1622 (7%) | 25/426 (6%) | 72/1084 (7%) | 16/112 (14%) | OR 1·06 (0·63 to 1·78) | OR 2·48 (1·12 to 5·48)* | |
| Personal care: problems with washing or dishing | 11/1622 (1%) | 0 | 10/1084 (1%) | 1/112 (1%) | NA | NA | |
| Usual activity: problems with usual activity | 25/1611 (2%) | 5/425 (1%) | 15/1076 (1%) | 5/110 (5%) | OR 1·10 (0·35 to 3·50) | OR 3·42 (0·74 to 15·78) | |
| Pain or discomfort | 431/1616 (27%) | 111/422 (26%) | 274/1082 (25%) | 46/112 (41%) | OR 0·86 (0·66 to 1·13) | OR 1·94 (1·19 to 3·16)* | |
| Anxiety or depression | 367/1617 (23%) | 98/425 (23%) | 233/1081 (22%) | 36/111 (32%) | OR 0·88 (0·66 to 1·17) | OR 1·77 (1·05 to 2·97)* | |
| Quality of life ‡ | 80·0 (70·0 to 90·0) | 80·0 (70·0 to 90·0) | 80·0 (75·0 to 90·0) | 80·0 (70·0 to 87·5) | β 2·68 (−1·55 to 6·91) | β −2·33 (−10·60 to 5·95) | |
| Distance walked in 6 min, m | 495·0 (440·0 to 538·0) | 495·0 (446·0 to 542·0) | 495·0 (439·0 to 537·0) | 479·0 (434·0 to 515·5) | β −9·25 (−18·80 to 0·26) | β −32·50 (−51·40 to −13·60) § | |
| Percentage of predicted value ¶ | 87·7 (75·9 to 101·1) | 87·8 (76·3 to 101·3) | 87·9 (76·3 to 101·5) | 85·2 (72·9 to 98·6) | β −1·58 (−3·59 to 0·43) | β −5·61 (−9·60 to −1·62)* | |
| Less than lower limit of the normal range ‖ | 392/1692 (23%) | 103/423 (24%) | 255/1153 (22%) | 34/116 (29%) | OR 1·13 (0·81 to 1·57) | OR 2·18 (1·18 to 4·03)* | |
| eGFR<90 mL/min per 1·73 m 2 | 487/1393 (35%) | 121/338 (36%) | 326/967 (34%) | 40/88 (45%) | OR 0·86 (0·63 to 1·19) | OR 1·44 (0·76 to 2·70) | |
研究人员对94名患者在感染急性期和发病6个月后的新冠抗体进行检测,与急性期相比,在发病6个月后患者体内中和抗体的滴度下降超过一半(52.5%)。也就是说,与急性期相比,发病6个月时新冠病毒中和抗体的水平下降明显,这带来了对患者愈后再次感染可能性的担忧。
国家呼吸医学中心、中日友好医院和首都医科大学的曹彬教授表示:“因为COVID-19是一种新发的疾病,我们才刚刚开始了解它对患者健康的长期影响。我们的随访研究表明,大部分患者在出院后仍然会继续受到该病毒的至少部分影响,出院后的医疗照护是非常有必要的,特别是针对住院时病情更重的患者。我们的研究也提示在更大的人群中进行更长期随访研究的重要性,以便了解该疾病可能对人体产生的全面影响。”
意大利马里奥·内格里药理研究所(Istituto di Ricerche Farmacologiche Mario Negri IRCCS)的专家Monica Cortinovis, Norberto Perico, 和 Giuseppe Remuzzi (并未参与此项研究)撰写了本研究的相关评论,对“COVID-19对健康可能产生的长期影响的不确定性”做出了评价。评论写道:“目前对COVID-19远期结局的研究报道较少,因此黄朝林和同事们的这项随访研究的发表非常及时且有重要意义。”
与本研究作者提出仍需进一步研究相呼应,意大利的专家们补充道:“尽管该研究对于COVID-19出院患者的结局进行了综合评估,但是最终纳入分析的研究对象只有4%的患者入住了重症监护室,因此本特定队列研究提供的信息对于COVID-19患者的长期结局并非盖棺定论。尽管如此,既往关于入住重症监护室后患者结局的研究表明,住院期间病情危重的新冠肺炎患者出院后将会出现认知功能和精神健康和/或身体功能方面的损伤,其损伤程度远远超过出院时。”
原始出处:
Chaolin Huang,Lixue Huang,Yeming Wang,Xia Li,Lili Ren,Xiaoying Gu,Liang Kang,Li Guo,Min Liu,Xing Zhou,Jianfeng Luo,Zhenghui Huang,Shengjin Tu,Yue Zhao,Li Chen,Decui Xu,Yanping Li,Caihong Li,Lu Peng,Yong Li,Wuxiang Xie,Dan Cui,Lianhan Shang,Guohui Fan,Jiuyang Xu,Geng Wang,Ying Wang,Jingchuan Zhong,Chen Wang,Jianwei Wang,Dingyu Zhang,Bin Cao.6-month consequences of COVID-19 in patients discharged from hospital: a cohort study. Lancet ,DOI:https://doi.org/10.1016/S0140-6736(20)32656-8
Monica Cortinovis,Norberto Perico,Giuseppe Remuzzi.Long-term follow-up of recovered patients with COVID-19


